Overview of anaphylaxis
- Anaphylaxis is an acute life threatening allergic reaction. Although many drugs can cause anaphylaxis reactions, the most commonly reported ones are penicillins, insulin, aspirin and other NSAIDs. Signs and symptoms involve the skin (e.g. flushing, pruritus, urticaria and angioedema), respiratory tract (e.g. tightness of the throat and chest, dyspnea, congestion, rhinorrhea and sneezing), gastrointestinal tract (e.g. nausea, cramping, vomiting and diarrhea) and cardiovascular system (e.g. hypotension and tachycardia).
- Anaphylactic shock generally begins within 30 minutes to 2 hours of exposure to the allergen. The risk of fatal anaphylaxis is greatest within the first few hours. Late phase of “ biphasic reactions “ can occur 1 hour to 72 hours after the initial presentation with most occurring within 10 hours. Because of the possibility of a biphasic reactions, patients should be observed for at least 12 hours after the anaphylactic reaction. Fatal anaphylactic shock most often results from asphyxia caused by airway obstruction either at the larynx or within the lungs. Cardiovascular collapse may occur as a result of asphyxia in some cases, in other cases cardiovascular collapse may be the dominant manifestation from the release of mediators within the heart muscles and coronary blood vessels.
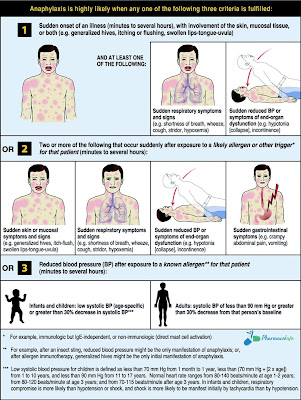
Criteria of diagnosis of anaphylactic shock
Anaphylactic
shock is highly likely when one of the following three criteria is present:
- Acute onset of reaction (minutes to several hours with invlovment of the skin, mucosal tissue or both (e.g. generalized hives “pruritus or flushing” , swollen lips, tongue or uvula) and at least one of the following:
- Respiratory compromise (e.g. dyspnea, wheezing, bronchospasm, reduced peak expiratory flow or hypoxemia).
- Reduced blood pressure or associated rapidly symptoms of end organ dysfunction (e.g. hypotonia, syncope or incontinence).
- Two or more of the following that occur rapidly after exposure to a likely allergen (minutes to several hours):
- Involvement of skin mucosal tissues (as mentioned above).
- Respiratory compromise (as mentioned above).
- Reduced blood pressure or associated symptoms (as mentioned above).
- Persistant gastrointestinal symptoms (e.g. abdominal cramps, vomiting).
- Reduced blood pressure after exposure to known allergen for that patient (minutes to several hours).
Summary of criteria of diagnosis of anaphylactic shock
Anaphylactic
shock is diagnosed if one of the following criteria is present:
- Sudden onset of skin manifestations and respiratory symptoms or cardiovascular symptoms.
- Sudden onset of 2 of the following after exposure to a likely allergen or other trigger: skin manifestations, respiratory manifestations, cardiovascular manifestations, gastrointestinal manifestations.
- Reduced blood pressure after exposure to a known allergen for that patient ( infants and children: low systolic B.P or greater than 30% decrease in systolic B.P , adults: B.P of less than 90 mmHg or greater than 30% decrease of B.P from that patient baseline).
Pharmacologic management of anaphylactic shock
Immediate intervention
Epinephrine (1
mg/mL):
- Adults: give 0.2-0.5 mg/kg intramuscularly, repeat every 5 minutes as needed.
- Children: give 0.01 mg/kg (maximum 0.3 mg/kg) intramuscularly, repeat every 5-15 minutes as needed.
Subsequent intervention
- Normal saline infusion “ fluid resuscitation “.
- Epinephrine infusion:
If the patient is not responding to epinephrine injections and fluid resuscitation.
Other considerations after epinephrine and fluids:
- Diphenhydramine I.V or I.M “ for rash and urticaria “.
- H2 blocker I.V “ for severe abdominal manifestations if present “.
- Inhaled Beta 2 agonist “ for bronchospasm resistant to epinephrine “.
- Dopamine I.V infusion “ for hypotension resistant to fluids and epinephrine “.
- Hydrocortisone I.V “ for severe or prolonged anaphylaxis “.
References
World allergy
organization guidelines for the assessment and management of anaphylaxis.


Comments
Post a Comment